Does Vitamin D Lessen COVID-19 Risk?

The headlines have been abuzz with the possibility that vitamin D could lessen the risks of COVID-19.
Much of the information has pointed out that the pandemic began in the Northern Hemisphere during winter. Down under things began in summer and we’ve seen notably better outcomes [so far]. Some say the virus doesn’t like the heat; others put it down to higher levels of vitamin D.
We include vitamin D3 in 55+ as it’s known to be critical to bone health – a big issue for menopausal women. However, among other things, it’s also proven to help with respiratory illness and the immune system.
Vitamin D & COVID-19
Since the advent of COVID-19 there has been a plethora of research into vitamin D. Scientists are investigating whether it is able to reduce the risk of infection and death with COVID-19.
At first, some schools of thought said yes, there’s an out and out link, others said not so much. The numerous published studies now completed show that vitamin D deficiency increases risk and outcomes.
- An early study was conducted by the Queen Elizabeth Foundation Trust and the University of Anglia in England. The research looked at 20 European countries and found vitamin D levels of patients with COVID-19 were ‘‘strongly associated’’ with how they fared.
- More recently, this research explored vitamin D’s ability to reduce viral replication and respiratory tract infections.
- The Irish Longitudinal Study (TILDA) at Trinity College in Dublin released a report on vitamin D and its relation to COVID-19 in response to the pandemic. Professor Rose Anne Kenny, Principal Investigator of TILDA, said:
‘‘We have evidence to support a role for Vitamin D in the prevention of chest infections, particularly in older adults who have low levels. In one study Vitamin D reduced the risk of chest infections to half in people who took supplements. Though we do not know specifically of the role of Vitamin D in COVID infections, given its wider implications for improving immune responses and clear evidence for bone and muscle health, those cocooning and other at-risk cohorts should ensure they have an adequate intake of Vitamin D. Cocooning is a necessity but will reduce physical activity. Muscle de-conditioning occurs rapidly in these circumstances and Vitamin D will help to maintain muscle health and strength in the current crisis.”
That’s not to say vitamin D is a cure-all or the answer to wiping out COVID. However, it does present a case to ensure we have good levels of it in our bodies.
Position Statement: Vitamin D and health in adults in Australia and New Zealand.
Sunshine & Vitamin D
Technically vitamin D is not a nutrient but a hormone. Rather than getting it through food, our main source comes from sunlight on our skin. During the warmer months, we get a good dose as we’re outdoors a lot. However, when it’s cooler we stay inside more (as we do in quarantine!) and our levels can reduce. While our bodies store vitamin D for some weeks/months our skin still needs sunlight to maintain optimum levels. A good half an hour of sunshine daily – until your skin begins to turn pink – is enough to promote vitamin D synthesis. This should serve up to 10,000-20,000 units.
Tip: Darker skins need longer exposure
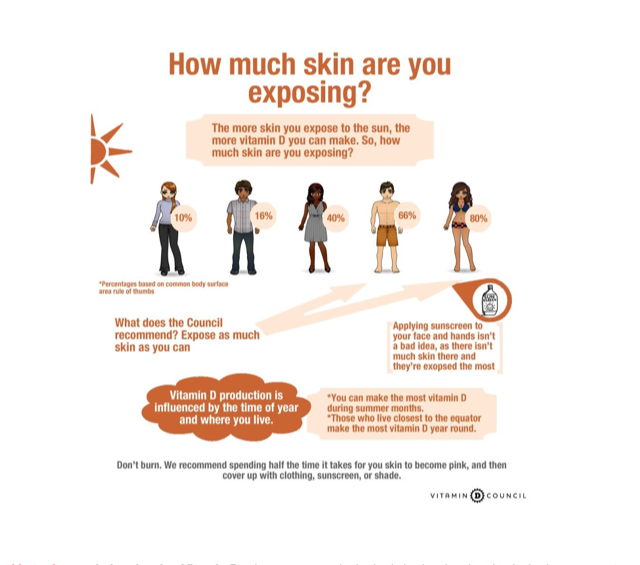
According to the Vitamin D Council in the US, when we’re in our winter clothes, we get 10 percent exposure. By comparison, when wearing a summer dress this increases to 40 percent and a bathing suit to 80 percent.
Food Sources Of Vitamin D
There are few food sources of vitamin D but you’ll find it in:
- Egg yolks
- Fatty fish like salmon, tuna and sardines
- Mushrooms grown in sunshine
- Cod Liver Oil
How Much Vitamin D Do We Need?
There are many differing opinions on this.
FYI: iu refers to international units.
Australia’s Health and Medical Research Council and New Zealand’s Ministry of Health recommend about 400 iu per day for women. For women aged over 50 this doubles. As we grow older we’re usually not outside as much and mature skin doesn’t synthesise vitamin D as well.
The general consensus for the optimum dosage is 800 iu per day. However, some experts say this is too low.
Leading authority Dr Michael Holick, author of The Vitamin D Solution recommends 1500-2000 iu for women per day. He believes insufficient vitamin D is the most common health problem we face today.
How To Get Your Vitamin D Levels Tested
- You can ask your doctor for a vitamin D test. When I requested one my GP told me they’re expensive and I would need to pay. But then I had an appointment with a rheumatologist who gave me one as a matter of course.
- There are home kits available as well. I’ve not used one but you can get them here in Australia, $49 AUD, and here in New Zealand. $75 NZD.
Vitamin D Deficiency
Deficiencies or low levels of vitamin D are linked to:
- Type 2 diabetes
- Depression
- Bone disease
- Hair loss
- Autoimmune diseases – Hashimoto’s, rheumatoid arthritis, fibromyalgia, chronic pain, multiple sclerosis
- And, perhaps, COVID-19
Dr Holick believes females should be particularly concerned about their vitamin D levels. He tells us that a deficiency can see us lose about 3-4 percent of our skeletal mass per year.
What he has to say below could be valuable for many of us. Indeed, I experienced debilitating chronic pain in the fascia (connective tissue around the bone) for five years. In my case, rheumatology could not get a diagnosis – the closest they got to was fibromyalgia or rheumatoid arthritis, which is wasn’t. I know many of you may relate on some levels. Interestingly, turning my diet around improved my symptoms by 80 percent.
“Women who suffer from aches and pains in their bones and muscles are often misdiagnosed as having fibromyalgia or chronic fatigue syndrome when in fact they are suffering from vitamin D deficiency. It is also recognised that women who had the highest intake of vitamin D reduced their risk of developing multiple sclerosis by 41 percent and rheumatoid arthritis by 44 percent. The Nurses’ Health Study at Harvard University revealed that women who had the highest intake of vitamin D reduced their risk of developing breast cancer by 50 percent.”
A Vital Vitamin
Vitamin D is vital for the health of our bones, brain, and heart and it’s why we include it in 55+. It performs best in combination with magnesium and that’s one of the reasons you’ll find magnesium in 55+ too.
- Taking your two capsules of 55+ per day gives you 600iu.
Vitamin D is also a great mood and sleep aid. In addition, science shows it strengthens our immune system and can help protect us against the flu.
Tip: A new study has found that vitamin D is 50% better absorbed when it is taken with food.
Please read this story too:
I hope this was helpful. Any questions fire them through here.
Main photo by Daoudi Aissa on Unsplashvir








